- 首页
- 关于我们
概况介绍 研究方向 人才培养 委员会/committee
- 员工团队
特聘专家 主要领导 行政团队 技术团队 PI团队- 科研平台
中心实验室 实验动物中心 生物样本库- 最新资讯
- 首页
- 关于我们
概况介绍 研究方向 人才培养 委员会/committee
- 员工团队
特聘专家 主要领导 行政团队 技术团队 PI团队- 科研平台
中心实验室 实验动物中心 生物样本库- 最新资讯
Dysbiosis and Implication of the Gut Microbiota in Diabetic Retinopathy发布日期: 2024-09-04
Abstract
The pathogenesis of type 2 diabetes mellitus (T2DM) is commonly associated with altered gut bacteria. However, whether the microbial dysbiosis that exists in human diabetic patients with or without retinopathy is different remains largely unknown. Here, we collected clinical information and fecal samples from 75 participants, including 25 diabetic patients without retinopathy (DM), 25 diabetic patients with retinopathy (DR), and 25 healthy controls (HC). The gut microbial composition in the three groups was analyzed using 16S ribosomal RNA (rRNA) gene sequencing. Microbial structure and composition differed in the three groups. The α and β diversities in both the DM and DR groups were reduced compared with those in the HC group. Blautia was the most abundant genus, especially in the DM group. In addition, increased levels of Bifidobacterium and Lactobacillus and decreased levels of Escherichia-Shigella, Faecalibacterium, Eubacterium_hallii_group and Clostridium genera were observed in the DM and DR groups compared with the HC group. Furthermore, a biomarker set of 25 bacterial families, which could distinguish patients in the DR group from those in the DM and HC groups was identified, with the area under the curve values ranging from 0.69 to 0.85. Of note, Pasteurellaceae, which was increased in DM and decreased in DR compared with HC, generated a high AUC (0.74) as an individual predictive biomarker. Moreover, 14 family biomarkers were associated with fasting blood glucose levels or diabetes, with most of them being negatively correlated. In summary, our study establishes compositional alterations of gut microbiota in DM and DR, suggesting the potential use of gut microbiota as a non-invasive biomarker for clinical and differential diagnosis, as well as identifying potential therapeutic targets of diabetic retinopathy.
相关文章-
Generation of vascularized retinal organoids containing microglia based on a PDMS microwell platformAbstractRetinal organoids (ROs) offer a biomimetic in vitro model for inves...2025-10-24
-
近期,爱尔眼科长沙医学中心陈建苏教授、唐仕波教授、崔泽凯副教授团队在角膜损伤修复和视网膜疾病治疗方面研究取得了多项令人瞩目的成果,为了解致盲性角膜和视网膜疾病的...2025-08-04
-
近日,由中国医师协会眼科医师分会遗传眼病学组牵头制定的《X连锁视网膜劈裂症临床诊疗的中国专家共识(2025)》(以下简称《共识》)正式发布。X连锁视网膜劈裂症是...2025-07-07
-
AbstractBackground Recent advances in clinical trials have involved the transpla...2025-05-06
-
Inherited retinal diseases (IRDs) can induce severe sight-threatening retinal de...2024-09-11
-
Corneal neovascularization (CNV) is a condition that can severely adversely affe...2024-09-05
-
Diabetic retinopathy (DR) is a common complication of diabetes and has a high pr...2024-09-04
-
Diabetic retinopathy (DR) development is associated with disturbances in the gut...2024-09-04
-
The three-dimensional (3D) retinal organoids (ROs) derived from human induced pl...2024-09-04
-
Tissue injury is a common clinical problem, which may cause great burden on pati...2024-09-04
-
Corneal nerve wounding often causes abnormalities in the cornea and even blindne...2024-09-04
-
Pre-mRNA processing factors (PRPFs) are vital components of the spliceosome and ...2024-09-04
-
Propagating large amounts of human corneal stromal cells (hCSCs) in vitro while ...2024-09-04
-
This study aimed to determine the effect of pinacidil, a nonselective KATP chann...2024-09-04
-
In vertebrates, most somatosensory pathways begin with the activation of dorsal ...2024-09-04
-
The pathogenesis of type 2 diabetes mellitus (T2DM) is commonly associated with ...2024-09-04
-
Corneal fibroblast can be transformed into corneal myofibroblasts by TGF-β1.2024-09-04
-
Age-related macular degeneration (AMD) is a common vision-threatening disease. T...2024-09-04
-
Suspended spheroid culture using ultralow attachment plates (ULAPs) is reported ...2024-09-04
-
本申请涉及细胞和器官培养技术领域,公开了一种三维类器官灌流培养器具,包括:细胞培养室,细胞培养室用于盛放培养基;多个换液槽,设于细胞培养室,用于更换细胞培养室中...2024-09-04
-
Purpose: Retinal inflammation is involved in the pathogenesis of several retinal...2024-09-03
-
Aging is a risk factor for multiple retinal degeneration diseases. Entraining br...2024-09-03
-
Angiographically silent cystoid macular edema (CME) is a rare complication from ...2024-09-03
-
The neuroretina is protected by its own defense system, that is microglia and th...2024-09-03
-
Purpose: We performed a bioinformatic transcriptome analysis to determine the al...2024-09-03
-
Previous research has shown that CXCR5−/− mice develop retinal degeneration (RD)...2024-09-03
-
Purpose: To investigate the levels of matrix metalloproteinases (MMPs) in aqueou...2024-09-03
-
In vitro generation of a functional retinal pigment epithelium (RPE) monolayer s...2024-09-03
-
We have established an induced pluripotent stem (iPS) cell line using urine-deri...2024-09-03
-
Purpose: The purpose of this study is to investigate the potential therapeutic b...2024-09-03
-
We report the human induced pluripotent stem cell line (iPSC) CSUASOi002-A, gene...2024-09-03
-
Background Central serous chorioretinopathy (CSC) is a widespread retinal disord...2024-09-03
-
Glaucoma is characterized by progressive, irreversible damage to the retinal gan...2024-09-03
-
Subarachnoid space (SAS) around optic nerve can be visible with swept-source opt...2024-09-03
-
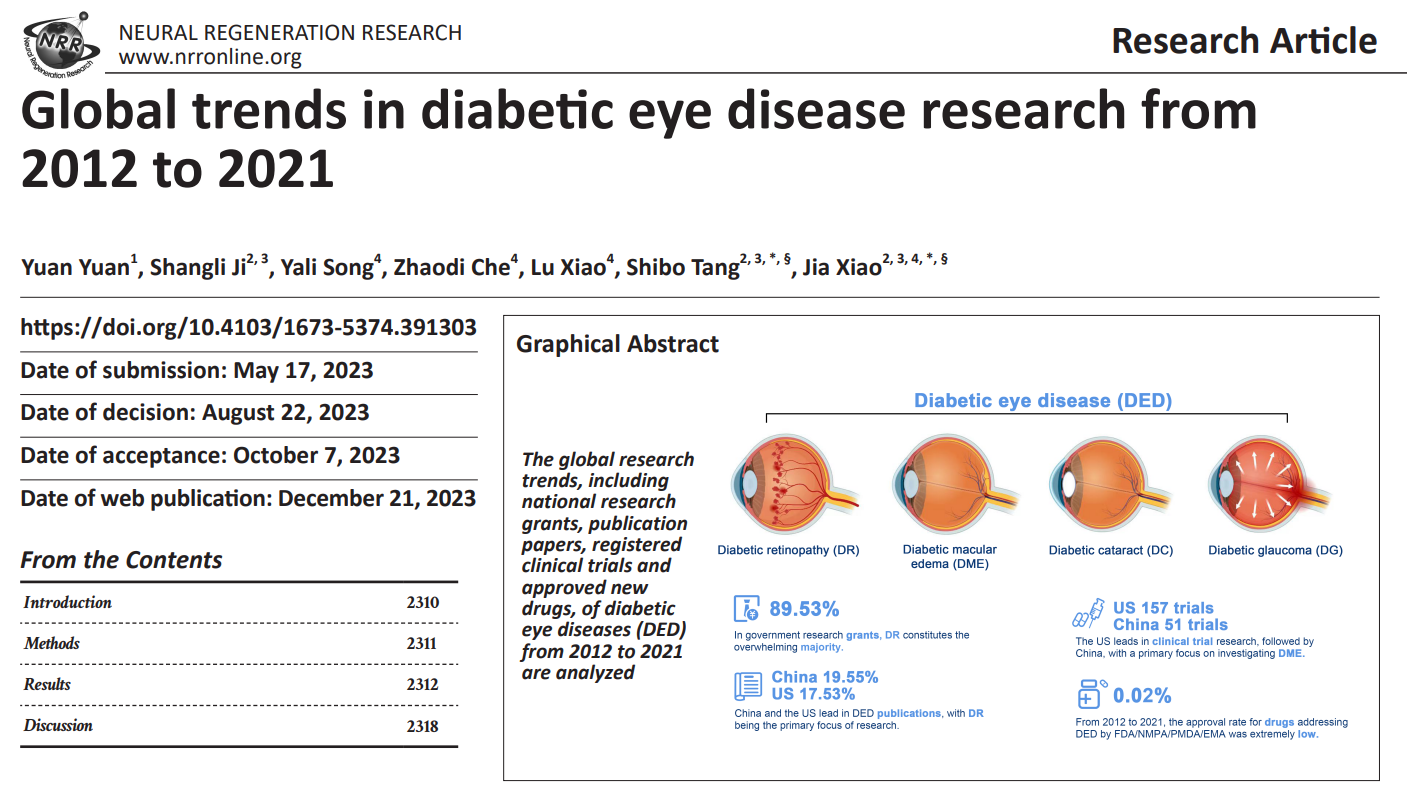
Diabetic eye disease refers to a group of eye complications that occur in diabet...2023-05-01
- 员工团队
- 员工团队